
According to world statistics, about 80% of adult inhabitants of our vast planet are united by the same health problem - periodically, or even constantly, back pain in the lumbar region. Lower back pain is the main symptom of many diseases of the spine and internal organs located in the abdominal cavity. And it is in vain that most of those who feel discomfort in this area, bypassing the doctor and not understanding the reasons, begin to intensively apply various ointments and other "homemade lotions". With these methods, you can easily achieve the opposite of the expected result.
Reasons: determine, exclude
The success of any treatment directly depends on the accuracy of the diagnosis, with the elimination of the symptoms experienced, the likelihood of relapse increases. Subsequently, such treatment can only aggravate the situation. Therefore, first of all, you need to carefully check the condition of all organs, the symptoms of which may be pain in the lumbar region.
Digestive system
Exacerbations of diseases of the digestive system (pancreatitis, ulcers, colitis, cholecystitis, enteritis, appendicitis) often provoke the appearance of pain in the lumbar region.

urinary system
Most often, kidney pain is confused with symptoms of diseases of the lumbar spine, since their nature is identical. Diseases of the kidneys and urinary tract of various etiologies are accompanied not only by a "recoil" in the lower back, but also by disturbances in urination (increased frequency, discomfort, presenceblood in the urine and its turbidity), and an increase in body temperature.
reproductive system
With problems with the reproductive organs in men and women in the acute stage, the pain often radiates to the lumbar region, tailbone or to the side. The nature of these pains is often belting without pronounced localization.
If a disease of an organ that is not associated with the musculoskeletal system is detected, then it is he who is treated, since it is he who is the real cause of the pain syndrome. If, after a thorough examination, problems with the above organs have not been identified, the problem is most likely in the spine.

Osteochondrosis
The most mobile part of the spine, which takes on most of the loads, is the lumbosacral. With a sedentary lifestyle, excessive stress and insufficient supply of nutrients to the cartilaginous tissues of the spine, degenerative-dystrophic changes in the intervertebral cartilage in the lumbar region occur - osteochondrosis.
Symptoms and stages of the disease
The main alarming symptom of osteochondrosis is pain in the lumbar region. At the initial stage, it is localized and directed to the sacrum, its character pulls (pain). During this period, destructive processes affected the nucleus pulposus (its dehydration occurs), as well as spinal discs (their standing height decreases). Discomfort is observed with heavy loads, and the pain itself is mild.
After a while, if the problem is ignored and no action is taken, shooting begins in the thigh and buttocks. Due to the narrowing of the intervertebral spaces, the muscles and ligaments "sag" and the spine becomes unstable. This leads to loss of sensation and numbness.
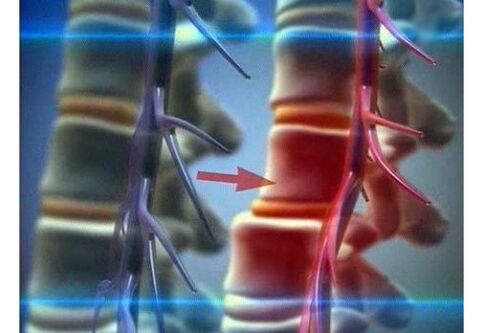
The third stage is characterized by morphological changes in the discs, the spine itself is severely deformed, disc protrusion and prolapse develop. The pain at this stage becomes more intense and prolonged. Every movement brings unbearable pain. It is possible to squeeze areas of the spinal cord, vessels and nerve endings adjacent to the sore spot due to the fact that the fibrous ring protrudes and affects the spinal canal.
The last stage of lumbar osteochondrosis "forces" the body to adapt to the changes that have arisen due to the disease in the following ways. In order for the supporting and protective functions to be preserved, bone tissue grows in the diseased area. This usually leads to various microtraumas, and then to disability.
Comprehensive treatment approach
Treatment of lumbar osteochondrosis must necessarily be comprehensive, regardless of the stage of the disease. With a mild form, the prognosis for treatment is favorable, deforming processes can be completely stopped, and the consequences minimized. At the last stage of the development of the disease, the task of treatment is to eliminate all symptoms and consequences, to normalize the nutrition of the spinal tissues, to strengthen the muscle corset of the entire back and its lower part in particular.
Medications
To relieve pain in lumbar osteochondrosis, painkillers are used in the form of tablets or injections, the second option is preferable, since it is more effective. To relieve the inflammatory process, anti-inflammatory drugs (non-steroidal) are prescribed. Muscle spasms that occur simultaneously with pain are eliminated by muscle relaxants. Chondroprotectors are used to restore damaged cartilage tissue.
All these remedies sometimes do not have the desired effect, since the damage prevents the drug from penetrating to the site of action.
The blockade is used to relieve an attack of acute pain. Only a specialist should do this.
A suitable painkiller is injected into the space between the spinous processes with a long needle. After such a procedure, the pain disappears very quickly, but for some time, since there is no therapeutic effect.
Effective use of local complex means - ointments, gels. They have an analgesic, anti-inflammatory, warming effect, many topical preparations contain a chondroprotector. These remedies, when used correctly and combined with massage, are quite effective.
Physiotherapy procedures
In combination with drug treatment of lumbar osteochondrosis, physiotherapeutic procedures are used - balneotherapy, laser and magnetotherapy, treatment with weak currents, light and vibration. They have practically no side effects and contraindications.
Alternative methods
Increasingly, alternative (non-traditional) methods are used simultaneously with traditional treatment - hirudotherapy, acupuncture, bee stings, manual therapy. These methods bring long-awaited relief, but some of them have contraindications, so consultation with the attending physician is necessary.
In addition to all the above methods of treatment, physiotherapy helps to overcome the disease. Properly distributed loads of the required intensity will help restore blood circulation in damaged areas, form or strengthen the muscle corset and thereby unload the spine.
In the treatment of osteochondrosis, it is important to correctly combine treatment methods, first of all, attacks of acute pain are relieved, then inflammatory processes, and only when the acute period of the disease is over, thenon-traditional methods and physical exercises can be used.
Yoga and Pilates complexes have proven to be excellent as rehabilitation programs for diseases of the spine.
Hernia of the lumbar spine
Against the background of undertreated or neglected osteochondrosis of the lumbar region, a hernia very often develops - a disease in which, due to insufficient physical activity or excessive load, the nutrition of the disc tissue becomesproduct, its strength decreases and, as a result, disc rupture. The process of destruction can drag on for many years and go unnoticed all this time, but with one unsuccessful movement the mechanism kicks in and all the symptoms begin to appear one after another.
General symptoms and course of the disease
Symptoms of a lumbar spine hernia include decreased tendon reflexes, pain of varying intensity, muscle weakness, and numbness in the extremities. Pain with a hernia does not always occur, back pain is possible, which gradually spreads in the direction of the pinched nerve.
Distortion of the body is a characteristic sign of a lumbar hernia. This phenomenon occurs involuntarily, because the body needs to find the most comfortable position in which the pain is minimal. In the event of a severe and rapidly progressive course of the disease, the consequences may be paralysis of the lower limbs (partial or complete). This phenomenon is usually accompanied by disturbances in the functioning of the abdominal organs, in particular the intestines and the bladder.
Clinical manifestations of a hernia of the lumbosacral zone are manifested by a constant increase in pain and its intensification during specific physical exertion (weightlifting, bending, sharp strong muscle tension, coughing), dull aching pain withlocalization in a point that does not disappear, the direction of pain in the buttock or leg, or numbness in this area.
Diagnosis of a hernia of the lumbar spine
It is difficult to diagnose a hernia visually or by the symptoms described by the patient alone. To more accurately determine the presence of the disease, several methods are used that will help to accurately determine the location of the disease. Computed tomography, nuclear magnetic and x-ray - thanks to these methods, the doctor will be able to visually determine the location of the pathologically altered vertebra and see the deformed disk.
To determine the severity of the disease and the consequences, doctors use several tests: straight leg lift, tendon reflexes, tenderness (reaction) of the leg at all levels (from the toes to the hip joint) at severaltypes of stimuli - pain, vibration and temperature.
Treatment methods
Depending on the severity and condition of the patient, different methods of hernia treatment are used. In the event of an exacerbation, first of all, it is necessary to immediately limit motor activity until bed rest and relieve pain with medication. After 5-7 days, when the acute period is over and the pain has subsided, drug therapy is supplemented with other restorative procedures (massage, physiotherapy, physical education).
Medical and conservative treatment of lumbar hernia is the same as for osteochondrosis.
Operation
In the case of a severe course of the disease and the presence of numerous serious consequences, surgical treatment is advisable.
Indications for surgery:
- sequestration of a hernia - part of the disc damaged by a herniation enters the spinal canal;
- dysfunction of all or one organ of the pelvis;
- the patency of the spinal canal is impaired (determined by MRI);
- lack of results when using a medical and conservative method of treatment for three months or more;
- inflammation of the sciatic nerve.
Surgical treatment of a hernia is now carried out using sparing and minimally invasive endoscopic operations.
The method of laser reconstruction involves the evaporation of fluid from the protruding nucleus pulposus using a laser. Thanks to this, the nerve root is "freed", that is, its compression is eliminated. But this type of intervention has a number of contraindications, these are early spinal operations, spondylolisthesis, spondyloarthritis, impaired spinal canal patency (stenosis) and protrusion of the nucleuspulposus in the canal.
To remove the damaged part of the intervertebral disc, the percutaneous discectomy method is used. Evaporation and removal of damaged tissue is performed with a needle inserted through the skin.
In the event that it is impossible to restore the damaged disc in any way, starting with medication and ending with a minimally invasive operation, or if all the methods used bring no results, the deformed disc is replacedby a prosthesis.
Preventive measures
In order to prevent the progression of the disease, special exercises are prescribed. Exercise complexes should be developed by a specialist individually for each patient and should contain exercises for muscle stretching, tension and light aerobic exercise.
With a hernia of the lumbar spine, doctors recommend wearing a special fixing belt. Outwardly it looks like a capsule, its width is about 30 cm, it is attached to the body with Velcro and has several degrees of rigidity.

This product is necessary to evenly distribute the load (from the diseased area to the healthy area) and relieve stress (unload). Injured segments of the spine with constant wearing of the belt are corrected and returned to their anatomical position.
Lumbodynia with radicular syndrome
Against the background of osteochondrosis and hernia of the lumbar spine, lumbago develops - lumbar back pain (sharp paroxysmal pain). This is the "simplest" scenario. Since hernias and osteochondrosis are characterized by deformation and frequent prolapse of the damaged disc and displacement of the spine, there is damage to nearby nerve roots, called radicular syndrome.
It is amplified by the involvement of the veins, which causes tissue edema (soft) and congestion. The symptoms of lumbodynia with radicular syndrome are similar to the symptoms of a lumbar hernia (sharp shooting pains that radiate downwards, loss of sensitivity and altered reflexes), and since this is a consequence, the cause mustfirst be treated with an integrated approach, otherwise disability threatens.
Sciatica
Another consequence of hernia and osteochondrosis is inflammation of the sciatic - sciatic nerve and the accompanying pain that radiates to the leg or buttock. Despite the ability to clearly define the "painful" place, the reason lies in the spine.
Sciatica is not an independent disease, this term refers to a number of symptoms that accompany certain diseases of the spine. The pain sensations can be different, in some cases it is just a slight discomfort when you stay in the same uncomfortable position for a long time, and sometimes the pain leads to loss of consciousness and painkillers in this case do notnot help.
For effective treatment, it is not enough to diagnose sciatica or lumbago, in any case, it is necessary to conduct a comprehensive comprehensive examination by various specialists and accurately identify the cause, because it is she whois the provoking factor. With the elimination of only some of the symptoms, the likelihood of progression of the underlying disease and the occurrence of many complications increases. A careful attitude to your health, early detection of problems and timely treatment are the key to good health.
















